1) Introduction
2) Respiration & Airway
Clearance (Cough)
3) Gastric Clearance & Colon
Transfer
4) Bladder Control
5) Deep Vein
Thrombosis
Introduction: Because nerves are electromagnetically driven
cells, it is not surprising that pulsed magnetic fields can initiate the
neuronal propagation of signals to paralysis-affected muscles.
Basically, this artificially initiated neural signal can stimulate
muscle contractions if activated on a motor nerve.
The use of magnetic fields to promote functional or
rehabilitative benefits is called functional magnetic stimulation (FMS).
In individuals with SCI, FMS has been used to stimulate breathing,
enhance digestion, control urination, speed bodily wastes through the
colon, and enhance circulation. (Other electromagnetic SCI applications
have been discussed previously).
Similar to functional electrical stimulation (FES)
discussed elsewhere, FMS requires that target muscles or organs are
innervated (peripheral nerves intact) to affect bodily functions and
muscle contractions. Like FES, FMS is applied below the injury level to
facilitate functions that have been lost or impaired.
FMS systems
consist of three components: a high-current pulse generator, magnetic
coil, and power source. FMS pulse generators discharge output currents
of 5,000 amps or more with pulse durations usually close to 250
microseconds. This high electrical output requires a powerful energy
source. Internal circuitry in the pulse generator includes a storage
capacitor that charges up to several thousand volts, control circuitry,
and a thyristor - a solid state device able to switch large amounts of
electrical current in a few microseconds.
To induce signal propagation, FMS magnetic coils
generate field strengths of two Tesla or more, a powerful
electromagnetic force (comparable to magnetic resonance imaging, i.e.
MRI). The magnetic coil (MC) typically consists of one or more
well-insulated copper coils, temperature sensors, and safety switches -
all housed in a molded plastic case. Either batteries or fixed
electrical sources are used to generate FMS.
Unlike FES, which applies electrical current
directly to the skin or nerves through external or implanted electrodes,
FMS affects nerve cells through a pulsed magnetic field, which radiates
from one or more magnetic coils placed outside the body over target
nerves, or nerve roots. This difference between FMS and FES presents
benefits and drawbacks.
Benefits include:
-
FMS penetrates
tissues, including skin, fat, and bone, reaching peripheral nerves,
the spinal cord, spinal nerve roots, the brain, and internal organs
without surgery.
-
FMS induces an
electric field under the area of application, providing a means for
simultaneous stimulation of multiple nerves. [Note: If the
functional stimulation of a muscle group is desired this property is
beneficial, whereas it can be a drawback if the activation of a
specific nerve or muscle is desired.]
-
FMS avoids risks
associated with surgically implanted FES electrodes.
-
FMS can be applied
over clothing; it does not require direct skin contact.
Drawbacks include:
-
FMS can activate
inappropriate nerves that lie within its field, because FMS radiates
a magnetic field rather than a focused electrical current.
-
Present FMS systems
can be unwieldy.
According to
Dr. Vernon Lin (USA),
 a
leading pioneer in FMS for SCI applications, two technical factors have
slowed FMS development for widespread home and clinical use – magnetic
coil-field dispersion and battery size. However, changes in magnetic
coil design are improving the ability to target specific nerves with
FMS. Likewise, improvements in battery technology are making portable
FMS a possibility for individual use. Although the small market
represented by potential FMS users coupled with its present costs are
slowing FMS commercial development, Lin believes that FMS will
eventually serve multiple SCI applications.
a
leading pioneer in FMS for SCI applications, two technical factors have
slowed FMS development for widespread home and clinical use – magnetic
coil-field dispersion and battery size. However, changes in magnetic
coil design are improving the ability to target specific nerves with
FMS. Likewise, improvements in battery technology are making portable
FMS a possibility for individual use. Although the small market
represented by potential FMS users coupled with its present costs are
slowing FMS commercial development, Lin believes that FMS will
eventually serve multiple SCI applications.
FMS APPLICATIONS FOR SCI
Respiration & Airway Clearance (Cough):
FMS breathing assistance may offer
benefits superior to those presently gained through FES. Early on, it
was shown that a magnetic coil placed over the cervical C7 vertebra
stimulates diaphragm-controlling phrenic nerves without surgery.
Compared to FES, FMS resulted in higher diaphragm pressures, which
researchers believe resulted from the activation of not only the phrenic
nerves but also nerves to upper chest-wall muscles.
Dr. Lin’s
investigative team examined the effect of FMS in conditioning the
muscles used for expiration (i.e. exhalation) in eight subjects with
SCI. Of these subjects, seven had cervical injuries ranging between the
C5 and C7 level, and one had a thoracic T5 injury. Subject age averaged
51 years, and the time lapsing since injury averaged 18 years. Each
subject received a four-week conditioning program consisting of a
20-minute, twice-daily FMS session five times per week. The magnetic
coil was placed at the T10-11 level while subjects were sitting in their
wheelchairs. This placement stimulates the lower intercostal and
abdominal muscles.
Pulmonary
functional assessments were carried before, in the middle of,
immediately after, and two weeks after the conditioning program. When
compared to baseline functioning, FMS treatment resulted in considerable
improvement in voluntary expiratory pressure (116%), volume (173%), and
flow rate (123%). However, two weeks after conditioning terminated,
these improvements receded to preconditioning levels, indicating that
persistent stimulation would be required if the patients were to benefit
over the long term.
Gastric
Clearance & Colon Transfer:
SCI can adversely affect the gastrointestinal tract, slowing the movement
of solids though the stomach and colon. Signs of a neurogenic bowel
include fecal impaction, constipation, abdominal distention, prolonged
bowel care, and delayed colonic transit. It has been estimated that
41-86% of individuals with SCI have some of these problems, and 41%
spend at least one hour daily on bowel care.
Dr. Lin and
associates demonstrated that FMS increases rectal pressures and shortens
colon-transfer time in individuals with SCI. This study was divided in
two protocols, the first designed to assess FMS’ impact on rectal
pressure and the second, FMS’ effect on colonic transit times. In the
first protocol, after carrying out preliminary, procedure-establishing
experiments in several able-bodied men, the investigators studied nine
men with both complete and incomplete injuries, ranging from the C3
cervical to lumbar L1 level. The MC was placed over the lower abdomen,
which tenses abdominal musculature, and then the lumbosacral region,
which stimulates colon- and rectum-controlling sacral nerves. With the
abdominal stimulation rectal pressure increased 42% and with lumbosacral
stimulation, 80%.
In protocol 2,
the colonic transit times were assessed in four individuals with SCI
before and after a five-week magnetic-stimulation period. Basically,
with these studies, subjects consumed with breakfast on the first three
days 20 radiopaque markers (i.e., shows up with x-ray), which are then
followed as they transit through the GI system. The five-week FMS
program consisted of twice daily 20-minute sessions that increased in
intensity over time. After the five-week treatment period, colonic
transit time decreased on average from 105 to 89 hours.
In a study
published the following year (2002), Lin and colleagues evaluated
gastric emptying with and without FMS in five able-bodied men and four
subjects with SCI (three men and 1 women). After fasting overnight for
12 hours, all subjects were fed a brea kfast
that included fried eggs with a radioactive tracer. Subjects laid down
face up with a radioactivity detector positioned over the abdomen and
the magnetic coil placed underneath at the T9-vertebral level. Thirty
minutes of on-off magnetic stimulation was administered. Although FMS
enhanced gastric emptying in all subjects, it especially accelerated the
process in individuals with SCI. Specifically, in able-bodied subjects,
FMS shortened gastric emptying by 8%; in contrast, in individuals with
SCI, FMS shortened emptying by 33%. In one subject with SCI, gastric
emptying was 38 minutes faster with FMS.
kfast
that included fried eggs with a radioactive tracer. Subjects laid down
face up with a radioactivity detector positioned over the abdomen and
the magnetic coil placed underneath at the T9-vertebral level. Thirty
minutes of on-off magnetic stimulation was administered. Although FMS
enhanced gastric emptying in all subjects, it especially accelerated the
process in individuals with SCI. Specifically, in able-bodied subjects,
FMS shortened gastric emptying by 8%; in contrast, in individuals with
SCI, FMS shortened emptying by 33%. In one subject with SCI, gastric
emptying was 38 minutes faster with FMS.
In a more
recent study with more subjects, Dr. Po-Yi Tsai
et al (Taiwan) further documented the benefits of FMS to enhance bowel
function after SCI. This study recruited 22 patients (19 men; 3 women)
averaging 47-years old and who had sustained their injuries on average
39 months earlier. The subjects were divided into subgroups, consisting
of those with lower-level and higher-level injuries. This distinction
was important because higher and lower level injuries affect
bowel-function physiology differently. As such, due to the nerves that
are stimulated by FMS, treatment efficacy could conceivably vary
considerably.
All subjects
underwent a three-week FMS program consisting of twice daily 20-minute
sessions. The magnetic coil was placed at the T9 vertebral level for the
first 10 minutes and then at the L3 level for 10 minutes. Bowel function
was measured before and after the program by 1) assessing colonic
transit time through following the progression of ingested radiopaque
markers, 2) a questionnaire ascertaining the patients’ impressions of
bowel function and health, and 3) telephone follow-up interviews every
other week for three months.
After the FMS
program, the average colonic transit time decreased from 63 to 50 hours.
Improvements in colonic transit were noted in both the higher-injury and
lower-injury groups. The before-and-after questionnaire also documented
bowel-function improvement. For example, improvements were noted in
frequency of laxative use, unsuccessful evacuation attempts, feeling of
incomplete defecation, difficulty with evacuation, and time taken.
Bladder
Control: Dr. Vernon Lin’s
investigative team showed that magnetic stimulation of the sacral nerves
could trigger urination in 17 of 22 subjects with SCI. The study found
that individuals with reflex or spastic bladders (spontaneously empty as
a reflex when filled) responded well to using FMS for bladder control.
Reflex bladders most often occur in individuals with higher spinal cord
lesions. FMS wasn’t as effective for individuals whose bladders did not
empty of their own accord (flaccid bladders).
Deep Vein Thrombosis:
With deep vein thrombosis (DVT), a
blood clot forms in a deep vein of the leg, pelvis or occasionally the
arm. This clot potentially can dislodge and travel to the lungs, where
it can create a life-threatening pulmonary embolism. Overall, the
reported incidence of DVT in SCI ranges from 47 to 72%. In the acute
phase of injury, the incidence is 13.6%, with risk dropping about 20
days after the injury. DVT is more common in patients with paraplegia
and in those with complete injuries.
Dr. Vernon Lin,
Dr. Ian Hsiao and colleagues evaluated the effect of stimulating leg
muscles with FMS on the break down of the blood-clotting protein fibrin
(i.e., a process called fibronolysis). In the clotting process, fibrin
molecules combine to form long strands that enmesh platelets, gradually
forming a mass that hardens into a clot.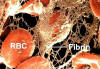 Specifically, the researchers
analyzed fibronolysis before and after 60 minutes of FMS-induced leg
contractions in 22 patients with SCI. The idea behind the research is
that promoting fibrin breakdown should lessen DVT risk. The
investigators concluded from the results that FMS produces “a sustained
enhancement of systemic fibronolysis that may prove useful in DVT”
prevention.
Specifically, the researchers
analyzed fibronolysis before and after 60 minutes of FMS-induced leg
contractions in 22 patients with SCI. The idea behind the research is
that promoting fibrin breakdown should lessen DVT risk. The
investigators concluded from the results that FMS produces “a sustained
enhancement of systemic fibronolysis that may prove useful in DVT”
prevention.
TOP